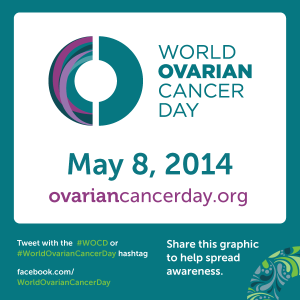
Each year, nearly a quarter of a million women around the world are diagnosed with ovarian cancer and the disease is responsible for 140,000 deaths annually. Statistics show that just 45% of women with ovarian cancer are likely to survive for five years compared with 89% of women with breast cancer. We ask that you join us on World Ovarian Cancer Day (May 8th) in the fight against the most lethal form of gynecologic cancer.
LEARN: World Ovarian Cancer Day — May 8, 2015
On May 8, 2015, the individuals from around the world are invited to join the global movement to raise awareness about ovarian cancer. This year the theme will celebrate the natural bond women have with each other, encouraging people to send in photos of celebratory bonding moments and to sign the awareness pledge located on the website (www.ovariancancerday.org) to spread the word about ovarian cancer for the third annual World Ovarian Cancer Day (WOCD).
Dr. Maya Soetoro-Ng, President Obama’s sister, speaks out about losing her mother to ovarian cancer.
“Now in its third year, World Ovarian Cancer Day has grown globally to over 78 organizations from 25 countries,” says Elisabeth Baugh, chair of the WOCD international organizing committee and CEO of Ovarian Cancer Canada. “In celebrating the unique bonds of women, we are acknowledging the strong drive they have to share and help each other. Without women, the world would not be. Joining together, our common voice symbolizes a global support group for the 250,000 women who will be diagnosed this year with ovarian cancer.”
Celebrate the women you love, trust, and are proud to know by helping to raise awareness about ovarian cancer and view a video of celebratory images to be released globally on May 8, World Ovarian Cancer Day.
“Our outreach has demonstrated the ability of this campaign to increase awareness of the disease and to connect people internationally with the resources available to educate others,” explained members of the Steering Committee, Calaneet Balas, CEO of the Ovarian Cancer National Alliance, Annwen Jones, Target Ovarian Cancer and Alison Amos, Ovarian Cancer Australia. “This year we want to put faces to that movement – faces of women who care about and support each other.”
In 2015, not only cancer organizations, but all interested groups who care about the health of women internationally are invited to register and partner with us. The pledge also engages individuals worldwide, empowering them with information about ovarian cancer and a quick and easy way to pass on the word about the disease.
All those who sign the World Ovarian Cancer Day pledge at www.ovariancancerday.org will receive an e-card on May 8 with ovarian cancer risk and symptom information. This card is to be passed along to at least five friends, who in turn will be encouraged to pass it along to their friends.
Each year, nearly a quarter of a million women around the world are diagnosed with ovarian cancer and the disease is responsible for 140,000 deaths annually. Statistics show that just 45% of women with ovarian cancer are likely to survive for five years compared with 89% of women with breast cancer. Women in developed and developing countries are similarly affected by ovarian cancer.
The recent disclosure by Angelina Jolie Pitt in a New York Times Op-Ed about prophylactic surgery to remove her fallopian tubes and ovaries because of a genetic predisposition for ovarian and breast cancer has put knowledge about your family history in the spotlight. Approximately 15%- 20% of cases of ovarian cancer are due to family history. This means having a close blood relation (mother, sister, daughter, grandmother, granddaughter, aunt or niece) on either your mother’s or your father’s side of the family who has had breast cancer before the age of 50 or ovarian cancer at any age.
In addition to sharing symptom and risk information, WOCD will also focus on prevention of ovarian cancer.
WOCD’s social media campaign includes the WOCD website (available in 4 languages: English, French, Portuguese and Spanish), Facebook, Twitter, YouTube and Pinterest. Activities in 2014 were highlighted in photos and through the pledge dissemination which reached over 15,000 people. This will continue to grow on May 8, including “lighting the world in teal” – the color that represents ovarian cancer.
World Ovarian Cancer Day has become a global movement in three short years. Uniting patient organizations globally, it has also sparked interest and involvement from healthcare professionals in countries around the world. This year, we celebrate the voice of women in making a difference as we unite and speak with one voice to raise awareness of ovarian cancer. Globally, rejoicing on our unique bond, we will ensure that no woman with ovarian cancer walks alone.
Please join us by signing the pledge form.
EDUCATE: Ovarian Cancer Facts:
Libby’s H*O*P*E* is dedicated to my 26-year old cousin, Elizabeth “Libby” Remick, who died from ovarian cancer in July 2008. Our mission is to educate ovarian cancer survivors and their families, as well as the general public, about ovarian cancer under the principle that “information is power.” The key to a significant reduction in deaths from ovarian cancer is early detection. Early detection is best achieved by having women listen to their bodies for the subtle, yet persistent, early warning signs & symptoms of the disease as described below. Together, we can raise money for a reliable early detection test, and ultimately a cure, for ovarian cancer.
Please take time to educate yourself with respect to the important ovarian cancer awareness facts provided below.
— Overview: Ovarian cancer causes more deaths than any other cancer of the female reproductive system. It is the fifth leading cancer cause of death among U.S. women.
— By the Numbers: In 2015, the American Cancer Society (ACS) estimates that there will be approximately 21,290 new ovarian cancer cases diagnosed in the U.S. ACS estimates that 14,180 U.S. women will die from the disease, or about 38 women per day. The loss of life is equivalent to 28 Boeing 747 jumbo jet crashes with no survivors every year.
— Early Warning Signs: Ovarian cancer is not a “silent” disease; it is a “subtle” disease. Recent studies indicate that some women may experience persistent, nonspecific symptoms, such as (i) bloating, (ii) pelvic or abdominal pain, (iii) difficulty eating or feeling full quickly, or (iv) urinary urgency or frequency. Women who experience such symptoms daily for more than a few weeks should seek prompt medical evaluation.
— Who’s Affected: Ovarian cancer can afflict adolescent, young adult, and mature women.
— Risk Reduction: Pregnancy, the long-term use of oral contraceptives, and tubal ligation reduce the risk of developing ovarian cancer. Recent research suggests that the most common form of ovarian cancer actually starts in the fallopian tubes. Any woman who is about to undergo gynecologic surgery may wish to discuss with her surgeon the possibility of having her fallopian tubes removed at that time.
— Importance of Family History: Women who have had breast cancer, or who have a paternal or maternal family history of breast cancer or ovarian cancer may have increased risk. Inherited mutations in BRCA1/BRCA2 genes increase risk. Women of Ashkenazi (Eastern European) Jewish ancestry are at higher risk for BRCA gene mutations. The incidence of ovarian ovarian cancer among Ashkenazi Jewish women is 1-in-40 versus 1-in-72 in the general population. Studies indicate that preventive surgery to remove the ovaries and fallopian tubes in women who possess a BRCA gene mutation decreases the risk of ovarian cancer.
— Genetic Couseling: If a woman has a family history of breast or ovarian cancer as described above, she may wish to seek genetic counselling. In fact, there is a recent shift in thinking that any woman with ovarian cancer should also seek genetic counselling as an important step for herself and other members of her family.
— Other Risk Factors: Other medical conditions associated with an increased ovarian cancer risk include pelvic inflammatory disease and Lynch syndrome. The use of hormonal replacement therapy has been shown to increase ovarian cancer risk. Tobacco smoking increases the risk of mucinous epithelial ovarian cancer. Heavier body weight may be associated with increased risk of ovarian cancer.
— Lack of a Reliable Early Screening Test: There is no reliable screening test for the detection of early stage ovarian cancer. Pelvic examination only occasionally detects ovarian cancer, generally when the disease is advanced. A Pap smear is used to detect cervical cancer, not ovarian cancer. However, the combination of a thorough pelvic exam, transvaginal ultrasound, and a blood test for the tumor marker CA125 may be offered to women who are at high risk of ovarian cancer and to women who have persistent, unexplained symptoms like those listed described above.
— Prognosis: If diagnosed at the localized stage, the 5-year ovarian cancer survival rate is 92%; however, only about 15% of all cases are detected at this stage, usually fortuitously during another medical procedure. The majority of cases (61%) are diagnosed at a distant stage, for which the 5-year survival rate is 27%.
— Survival Statistics: The 5-year and 10-year relative survival rates for all disease stages combined are only 45% and 35%, respectively. However, survival varies substantially by age; women younger than 65 are twice as likely to survive 5 years as women 65 and older (58% versus 27%).
Please help us to (i) spread the word about the early warning signs & symptoms of ovarian cancer, and (ii) raise money for ovarian cancer research. The life you save may be your own or that of a loved one.
FIGHT: The “Holy Trinity” of Major U.S. Ovarian Cancer Organizations
There are three major U.S. ovarian cancer organizations that are working to increase ovarian cancer awareness, and/or raise money to fight the disease. They are listed below. Please consider making a donation to one or more of these critically important nonprofit organizations.
- Ovarian Cancer Research Fund
The Ovarian Cancer Research Fund (OCRF) is the largest independent organization in the U.S. that is dedicated exclusively to funding ovarian cancer research– and to finding a cure. Through its three research programs, OCRF funds many of the best researchers and the most innovative projects.
Since 1998, OCRF has awarded 63 leading medical centers 195 grants for ovarian cancer research: an investment totaling over $50 million. OCRF researchers are taking on ovarian cancer from many angles:
— Developing innovative strategies for early detection;
— Discovering genetic polymorphisms that increase risk for ovarian cancer;
— Understanding the underlying genetics and molecular biology of ovarian cancer;
— Identifying new, better targets for treatment;
— Determining how to super-charge a woman’s immune response to better fight ovarian cancer; and
— Deciphering how and why ovarian cancer spreads, and how to stop it.
You can click here to make a donation to OCRF through the Libby’s H*O*P*E*’s donation page.
- Ovarian Cancer National Alliance
The Ovarian Cancer National Alliance (OCNA) is one of the foremost advocates for women with ovarian cancer in the U.S. To advance the interests of women with ovarian cancer, OCNA advocates at a national level for increases in research funding for the development of an early detection test, improved health care practices, and life-saving treatment protocols. OCNA also educates health care professionals and raises public awareness of the risks and symptoms of ovarian cancer.
To make a donation to OCNA, click here.
- National Ovarian Cancer Coalition
The mission of the National Ovarian Cancer Coalition (NOCC) is to raise awareness and promote education about ovarian cancer. NOCC is committed to improving the survival rate and quality of life for women with ovarian cancer.
Through national programs and local Chapter initiatives, the NOCC’s goal is to make more people aware of the early symptoms of ovarian cancer. In addition, the NOCC provides information to assist the newly diagnosed patient, to provide hope to survivors, and to support caregivers.
To make a donation to NOCC, click here.
INSPIRE: Everyday Heroes in the Fight Against Ovarian Cancer.
Nearly 250,000 women are diagnosed with ovarian cancer every year around the world, and the disease also affects their families and friends. Please take time to visit the WOCD website and read the inspirational stories about survivors, volunteers, and family members who are overcoming ovarian cancer, as well as the endeavors people are taking on to raise awareness about the disease.
At Libby’s H*O*P*E*, we are amazed each and every day by the inspirational ovarian cancer survivors and family members that we hear about, correspond with, or meet. The stories below represent a small sample of incredible individuals who have successfully fought the disease, as well as those who are currently fighting the disease with courage and grace. There are also stories about women who have died from ovarian cancer, but contributed to ovarian cancer awareness in a unique and special way during life. In addition, there are stories about doctors, advocates, and other inspirational individuals who are clearly making a difference in the fight against the disease.
— “Bald is Beautiful,” March 20, 2008.
— “Patty Franchi Flaherty Loses Battle to Ovarian Cancer, But Deserves a Long Standing Ovation,” August 19, 2008.
— “Oscar Winner Kathy Bates Is an Inspirational Ovarian Cancer Survivor,” February 25, 2009.
— “Rare Form of Ovarian Cancer Not Getting Inspirational 13 Yr. Old Down; You Can Help!,” February 26, 2009.
— “Meet Laurey Masterton, 20-Year Ovarian Cancer Survivor Extraordinaire,” March 20, 2009.
— “The Rock Band ‘N.E.D.’: Their Medical Skills Save Many; Their Music Could Save Thousands,” March 29, 2009.
— “A Wish To Build A Dream On,” May 3, 2009.
— “Husband’s Love For Wife Inspires A 9,000 Mile Bike Trek To Raise Money For Ovarian Cancer Awareness & Cancer Prevention,” May 14, 2009.
— “Gloria Johns Was Told ‘Ovarian Cancer Patients Don’t Live Long Enough … To Have Support Groups;’ She Proved Otherwise,” June 5, 2009.
— “Vox Populi:* How Do Your Define “Tragedy?“, January 22, 2010.
— “Smile, Open Your Eyes, Love and Go On,” July 28, 2010.
— “PBS Documentary, ‘The Whisper: The Silent Crisis of Ovarian Cancer,'” September 21, 2010.
— “Determined Teen Loses Ovarian Cancer Battle, But Her Courage Inspires An Entire Community,” December 28, 2010.
— “Mrs. Australia Quest Finalist Veronica Cristovao Is Raising Ovarian Cancer Awareness ‘Down Under'”, February 28, 2011.
— “Whither Thou Goest, I Will Go …”, July 28, 2012.
— “Crowd Funding:” Paying Medical Bills With a Little Help From Your Friends (and Strangers Too!), January 17, 2013.
___________________________
For more information on World Ovarian Cancer Day visit: www.ovariancancerday.org
Facebook: www.facebook.com/WorldOvarianCancerDay
Twitter: @OvarianCancerDY
Pinterest: @OvarianCancerDY
Each participating country is linked through the dedicated website which has been established for World Ovarian Cancer Day. To find out more about activities in each country, please contact the local organization directly through the website at http://www.ovariancancerday.org/get-involved/